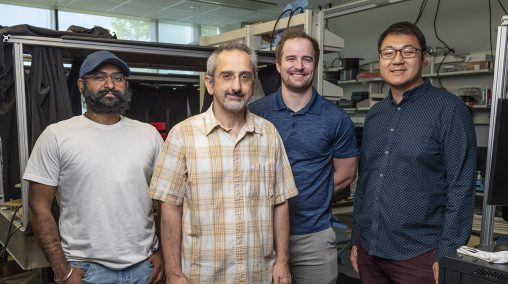
Ulas Sunar, Ohio Research Scholar and Endowed Chair in Medical Imaging, second from left with engineering graduate students, Dharminder Langri, left, Benjamin Rinehart, second from right, and Chien Poon.
Ulas Sunar, Ph.D., an Ohio Research Scholar and Endowed Chair in Medical Imaging at Wright State University, has received an $811,410 federal grant to develop a novel neuromonitoring approach for monitoring patients with acute brain injuries in neurointensive care units.
This is a special two-year R01 grant from the National Institute of Biomedical Imaging and Bioengineering in the National Institutes of Health, as part of the U.S. Brain Initiative, which is aimed at revolutionizing the understanding of the human brain by accelerating the development and application of innovative technologies.
The goal of Sunar’s grant is to develop a novel optical technology that provides blood flow measurements with higher sensitivity to brain tissue.
“Acute brain injuries can lead to secondary brain damage that worsens the outcome,” Sunar said. “Reduced cerebral blood flow can induce ischemia, while excess blood flow can cause hemorrhage. Therefore, there is a need for non-invasive, bedside, continuous cerebral blood flow monitoring approaches in neurointensive care units.”
Sunar is the director of the Biomedical Imaging Laboratory and an associate professor in the Department of Biomedical, Industrial and Human Factors Engineering in the Wright State College of Engineering and Computer Science.
Sunar’s team consists of Wright State graduate research students Chien Poon, Benjamin Rinehart and Dharminder Langri.
Sunar is collaborating with Brandon Foreman, M.D., an associate professor of neurology at the University of Cincinnati. Foreman, who has expertise on diagnosing and treating of patients with traumatic brain injury, will provide feedback for clinical translation. Consultant Lili He, Ph.D., an associate professor of radiology at Cincinnati Children, will provide feedback and support for the implementation of fast deep-learning algorithms. Yang Liu, Ph.D., assistant professor of statistics at Wright State, will provide statistical analysis support.
The researchers are working to develop a non-invasive method for cerebral blood flow monitoring that could be a safer alternative to traditional methods.
“In some neurointensive care units, cerebral blood flow is measured to monitor intracranial pressure. However, this method is invasive and requires drilling a burr hole through the skull, increasing the risk of hemorrhage and infection. Our non-invasive approach can replace invasive monitoring and serve as a quantitative clinical tool for longitudinal monitoring of neurological diseases,” Sunar said.
The researchers published their preliminary results in the journal Brain Sciences, demonstrating that non-invasive blood flow measures correlate well with invasive monitoring in a patient with traumatic brain injury.
Sunar plans to extend the study by improving the approach, including taking ultrafast measurements and increasing sensitivity to the brain.
“When you shine low-energy, picosecond pulsed light, photons pass through the skull, travel inside the brain, and then arrive back to the light detector,” Sunar said. “Our approach timestamps each photon so that information about their arrival times can be obtained. Early arriving photons travel small paths like the scalp, while late photons travel deep into the brain, and that is why they come back late. This concept is like a radar or sonar operation principle; time difference is related to the depth or distance of the target. We are interested in tardy photons since they most likely travel from the deeper brain tissue.”
Sunar’s team plans to utilize this optical approach to monitor many other types of brain injuries, such as ischemic stroke and hemorrhage, to guide and optimize treatment in settings of neurointensive care units.
“The proposed system can have a significant impact on a much larger population, including children and newborns, and it can have a broader impact on functional neuroimaging applications such as objective evaluations of human performance and neurofeedback,” Sunar said.

 Wright State names Rajneesh Suri dean of Raj Soin College of Business
Wright State names Rajneesh Suri dean of Raj Soin College of Business  ‘Only in New York,’ born at Wright State
‘Only in New York,’ born at Wright State  Wright State president, Horizon League leaders welcome new commissioner
Wright State president, Horizon League leaders welcome new commissioner  Wright State celebrates homecoming with week-long block party
Wright State celebrates homecoming with week-long block party  Wright State baseball to take on Dayton Flyers at Day Air Ballpark April 15
Wright State baseball to take on Dayton Flyers at Day Air Ballpark April 15 